Rehabilitation medicine is one of few specialities in which you can truly practice holistic medicine. You use your high-level medical knowledge and skills, setting them in the context of the patient as a whole person – their family and friends, their work and other interests and passions, their home and the area they live in, and their ambitions, hopes and fears. You work within a multi-professional team as an equal member of the team.
Your contribution is your detailed knowledge of disease. Your special skill is in understanding how disease interacts with all other aspects of the person, and in using this understanding to help the team and the person achieve the best outcome possible. You will work across all boundaries and with all agencies and professions. All your life you will be learning from other knowledgeable and skilled people. As a doctor, you may often lead the team, but this is not a right or expectation. Leadership must be learned, and the position must be earned.
As a consultant in rehabilitation medicine, you will face interesting and new challenges every day of your life – medical, ethical, legal, personal, and inter-personal. Because you are working closely with patients and their families, and with members of your team and other teams, you are always having to learn, to explain, to draw on your medical knowledge and skills. You also realise how much research is needed, and for anyone with an academic or research interest, the opportunities are huge.
Rehabilitation medicine - trainee characteristics
Rehabilitation medicine should be attractive to any doctor who:
- values and enjoys talking to and sharing expertise with patients and their families
- is comfortable with acknowledging uncertainty, and allowing patients to choose
- values and enjoys discussing clinical matters within a multi-professional team, as an equal member of the team, both learning from them and teaching
- wants life-long variety in their daily work
Working/training in an ST3 rehabilitation medicine post
Rehabilitation crosses all boundaries, and as a trainee you will learn how to act as a doctor in a great variety of settings, from intensive care units and specialist wards, through almost all specialist and generalist wards in hospitals, and through mental health settings, on to community settings such as nursing homes, day centres and patients’ homes.
The clinical workload in the UK used to focus on patients with any and all neurological disorders, including traumatic brain and spinal cord injury; trauma, including complex musculo-skeletal injuries and limb loss; other causes of limb loss; chronic pain including back pain; other more specific musculo-skeletal disorders; and a wide-range of psychologically-based problems alone or associated with a specific disorder.
However, rehabilitation benefits all patients, and with the new, 2021 curriculum (see link under Further Information), training also covers psychiatry and learning disability; cardiac and chest conditions; children and the elderly; renal services and so on. The scope of rehabilitation in the UK is now across all areas. The broad scope and experience of Rehabilitation Medicine has allowed it to take a leading role in managing the problems seen after Covid-19.
Rehabilitation Medicine knowledge and skills apply to all people receiving health care. You will learn about the nature and utility of the biopsychosocial model of illness; establishing patient priorities and negotiating team-based goals; liaising with other teams and professions; and having good medical diagnostic and treatment skills to recognise new problems, and to place each patient’s medical problems in the correct perspective.
The knowledge and skills applies to all people receiving health care. You will learn about the nature and utility of the biopsychosocial model of illness; establishing patient priorities and negotiating team-based goals; liaising with other teams and professions; and having good medical diagnostic and treatment skills to recognise new problems, and to place each patient’s medical problems in the correct perspective.
The changing nature of healthcare with increasing numbers of people with complex, long-term disabling disorders will require many rehabilitation medicine specialists. The increasing numbers of people with multiple morbidity, and with long-term disabilities coupled with the increasing emphasis on community healthcare gives this speciality a (potential) central place in healthcare this century. Join it.
See (freely available):
Wade DT, Halligan PW
The biopsychosocial model of illness: a model whose time has come.
Clinical Rehabilitation 2017;31:995-1004
Wade DT
Rehabilitation – a new approach: Overview and part one: the problems
Clinical Rehabilitation 2015;29:1041-1050
Wade DT
What is rehabilitation? An empirical investigation leading to an evidence-based description
Clinical Rehabilitation. 2020;34(5):571-583
Broad remit - team-based role
The physician works within a multi-professional team utilising his or her clinical and leadership skills, ability to assess risk, and emotional intelligence to manage patients in a goal-orientated rehabilitation programme.
This wide remit combines clinical skills and practice with the prospect of developing and implementing service improvements, teaching and training members of the multi-professional team, and promoting evidence-based rehabilitation through local and national policy.
Using existing expertise
Rehabilitation welcomes and greatly benefits from people with experience of and expertise in almost any medical (including surgical) specialty. Rehabilitation medicine is a small, but expanding, specialty and it is an excellent time to contemplate this progressive career choice. Training typically consists of a four-year programme, which encompasses learning across the clinical areas.
Competition levels
Competition ratios for ST3 posts are particularly favourable and diversity in applicants is welcomed with access to the programme being attainable after achieving almost any core training (see JRCPTB Rehabilitation Medicine site, link below).
Rehabilitation is increasingly becoming the focus of effective patient management and in recognition of this consultant posts are predicted to expand in the coming years.
Rehabilitation medicine is a bright, exciting specialty especially suited to doctors able to ‘think outside the box' and who wish to work predictable hours with manageable on-call commitments.
Further information
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty. The lead recruiter for rehabilitation medicine is West Midlands.
| NHS England West Midlands | ||||||
|---|---|---|---|---|---|---|
| email address | [email protected] | |||||
| website | www.westmidlandsdeanery.nhs.uk/ | |||||
Group 2 specialty
This is a Group 2 specialty and requires completion of the first two years of the internal medicine training (IMT) stage 1 programme or equivalent. Please visit the am I eligible? section of this website for further information about the eligibility criteria for Group 2 specialties.
Please be aware that this specialty accepts applicants from several other training routes, in addition to core-level physician training: anaesthetics, general practice, obstetrics and gynaecology, opthalmology, paediatrics, psychiatry, surgery.
Non-physician applicants must have obtained the basic specialty professional examination in addition to specific clinical experience and competences to be eligible.
Please view the specialty's person specification for information about the requirements for applying from a non-physician background and the deadlines for when this must be achieved.
Commitment to specialty
The specialty will be assessing your commitment to specialty as part of the shortlisting process. Please visit the application scoring page for more information about how this is assessed and scored.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
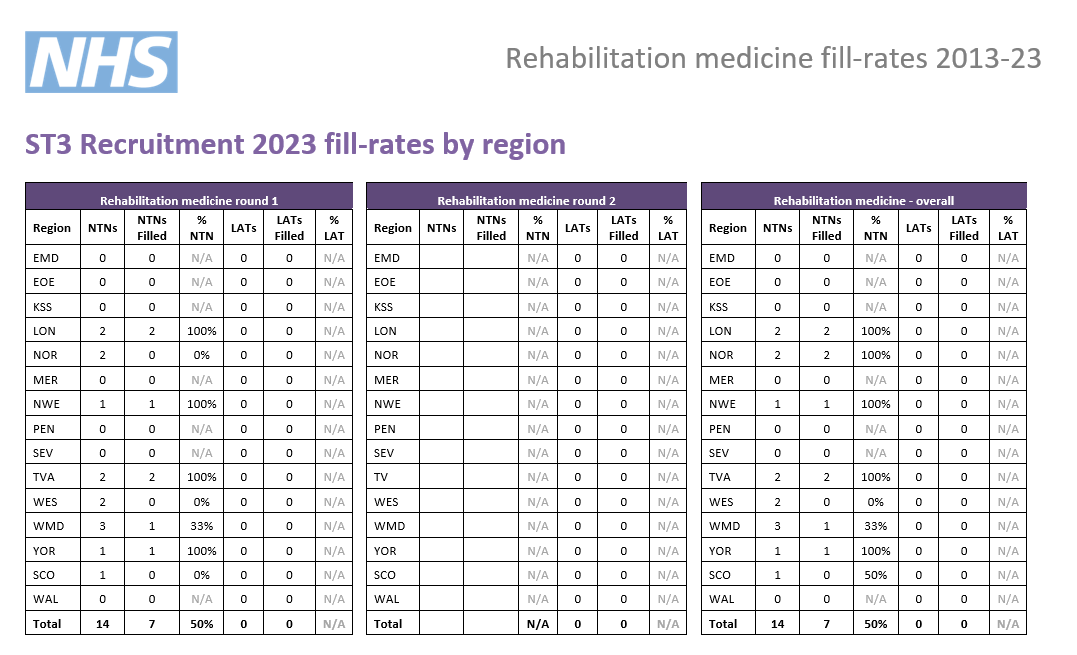
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts |
LAT posts |
Total posts |
Comp. | Unique* |
| 2023 | 41 | 14 | 0 | 14 | 3 | 44% |
| 2022 | 38 | 12 | 0 | 12 | 3.2 | 39% |
| 2021 | 42 | 14 | 0 | 14 | 3 | N/A |
| 2020 | 35 | 27 | 0 | 27 | 1.3 | 40% |
| 2019 | 19 | 25 | 0 | 25 | 0.8 | 32% |
| 2018 | 39 | 33 | 0 | 33 | 1.2 | 67% |
| 2017 | 34 | 21 | 0 | 21 | 1.6 | 32% |
| 2016 | 30 | 19 | 0 | 19 | 1.6 | 40% |
| 2015 | 36 | 22 | 1 | 23 | 1.6 | 50% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties)
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
| 2023 | |||||
| 2022 | 20 | 7 | 0 | 7 | 2.9 |
| 2021 | 35 | 14 | 0 | 14 | 2.5 |
| 2020 | 31 | 14 | 0 | 14 | 2.2 |
| 2019 | 12 | 19 | 0 | 19 | 0.6 |
| 2018 | 13 | 20 | 0 | 20 | 0.7 |
| 2017 | 12 | 20 | 0 | 20 | 0.6 |
| 2016 | 14 | 10 | 0 | 10 | 1.4 |
| 2015 | 8 | 12 | 1 | 13 | 0.6 |
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 interview dates & posts
| Region |
NTN posts
|
LAT posts*
|
Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
| West Midlands | 0 - 1 | N/A |
20/12/23 - 08/01/24
|
7, 8 March 2024
|
| East Midlands | 1 - 2 | N/A | ||
| East of England | 0 - 2 | N/A | ||
|
London |
0 |
N/A | ||
|
Kent, Surrey and Sussex |
0 |
|||
| North East | 0 - 2 | N/A | ||
| North West | 0 - 1 | N/A | ||
| South West |
Peninsula
0
|
N/A | ||
|
Severn
0 - 1
|
N/A | |||
| Thames Valley | 0 - 3 | N/A | ||
| Wessex | 1 - 3 | N/A | ||
| Yorkshire & Humber | 1 - 2 | N/A | ||
| Scotland** | 1 |
TBC
|
||
| Wales | 0 - 1 |
TBC
|
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
Interview content
The interview be split across two separate stations with a separate pair of interviewers scoring you on the areas within their station. There will be four questions, 8-10 minutes each in length. You will be marked on these questions, giving four scored areas in total. The headings below show the question areas and in which station they will be covered, along with information about what will be assessed.
Each station will last 18 minutes, so including the time between stations, the interview will be approximately 45 minutes.
Please note that this is subject to change and will be confirmed by the date of interview.
Prior to this question you will be given a clinical scenario and short while to review it. You will then be asked questions relating to this scenario. This question will last approximately 8 minutes.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Clinical scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario
You should also consider any other factors you deem appropriate, using your experience and professional judgement.
This discussion will be prompted by a short question (often a single sentence) provided by interviewers. This will not be given to you before discussion, this will be given verbally by interviewers once the previous question is finished. This question will last approximately 10 minutes.
This section of the interview is designed to assess your demonstration and understanding of professionalism and governance in a given situation.
Familiarise yourself with Good Medical Practice
Please note - assessment for this question is underpinned by the principles of GMC Good Medical Practice.
This question will see you given an ethical scenario to review As with the clinical scenario in question 1, this ethical scenario takes the form of a hypothetical situation, described briefly in text form, details of which will be given to you before answering the question. You will have a short while to review the scenario and there will be approximately 8 minutes of discussion afterwards.
This scenario focuses less on a clinical situation, and deals more with consideration of the moral, ethical, legal (etc.) issues which may arise in a situation.
The area of assessment here will be your suggested responses to the ethical scenario during discussion, as well as your knowledge of the different considerations required.
This question will focus on your suitability for and commitment to training in the specialty and give you opportunity to expand on the information provided in your application form.
This question will last approximately 10 minutes.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all eight scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 8 and 40.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your eight interview scores can be 1/5
- no more than two of your eight interview scores can be 2/5
- your RIS must be 24 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table accessible through the link below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
2.5 |
25 |
|
Question 2 |
||||
|
Professionalism and governance |
/ 5 |
/ 5 |
1.2 |
12 |
|
Question 3 |
||||
|
Ethical scenario |
/ 5 |
/ 5 |
1.8 |
18 |
|
Question 4 |
|
|||
|
Suitability and commitment |
/ 5 |
/ 5 |
2.5 |
25 |
|
Raw interview score |
/ 40 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 50 |
0.4 |
/ 20 |
|
|
Total score |
/ 100 |
|||